Abstract
Introduction
Chronic lymphocytic leukemia(CLL), characterized by monoclonal CD5+ B cells appearing in blood, marrow and lymphoid tissues, is the most common chronic leukemia in western countries. Until now CLL remains incurable with a heterogeneous clinical course, some patients developing progression rapidly while the others presenting a relatively indolent course. It has been reported that higher percentage of prolymphocytes was associated with increasing refractoriness to treatment and worse prognosis. In this study we were trying to explore the effect of prolymphocytes on the prognosis of CLL.
Methods
Two hundred and fifty-one treatment naïve CLL patients in Jiangsu Province Hospital were retrospectively enrolled in our study from April 2014 to November 2019. The median time from diagnosis to peripheral-blood smear examination was 0.13 month and median follow-up time was 30.87 months.
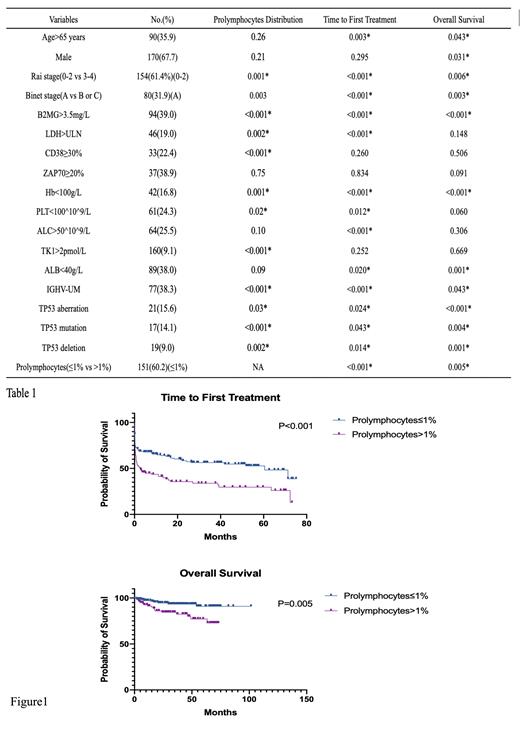
A total of 200 lymphocytes and prolymphocytes were counted. The percentage of prolymphocytes was collected. Basic clinical characteristics and other prognostic markers including age, sex, Rai and Binet stage, B2-microglobulin(B2MG), lactate dehydrogenase(LDH) level, CD38 and ZAP70 expression level, hemoglobulin(HB), platelets count(PLT), absolute lymphocyte count(ALC), thymidine kinase-1(TK-1), albumin(ALB), IGHV mutation status and TP53 status were also put in the analysis. The time to first treatment(TTFT)was defined as the time from sampling to first treatment and the overall survival(OS) time was the time from sampling to death.
An X-tile analysis provided the optimal prolymphocyte cutoff point. Wilcoxon rank sum test was used to compare the distribution of prolymphocytes percentage in different subgroups. The Kaplan-Meier method was used to construct the survival curves and the log-rank test was used to compare the difference. Multivariate analysis was conducted based on the Cox-regression model. All tests were two-sided and P<0.05 was considered to be statistically significant. Statistical analysis was performed with SPSS (version 26.0; IBM Corporation, Chicago, IL) and survival curves was drawn with GraphPad Prism (version 9.0: GraphPad Software, Inc., La Jolla, CA, USA).
Results
Among 252 patients, most of them were male(67.7%) and 35.9% were older than 65 years old. We found significantly different distribution of prolymphocytes percentage in patients with different B2MG, Rai stage, LDH, CD38 expression, TK1, IGHV mutation status and TP53 status(Table 1). The optimal cutoff of prolymphocytes percentage provided by X-tile analysis was 1%. Then all the patients were divided into two groups based on the prolymphocytes percentage and obvious survival difference between the two groups was shown in both TTFT(P<0.001) and OS(P=0.005)(Figure 1). Age, Rai stage, Binet stage, B2MG, LDH, ALC, ALB, IGHV mutation status and prolymphocytes percentage were further included in a multivariate analysis in which, however, prolymphocytes percentage didn't show an independent prognostic effect on TTFT(P=0.370, HR=1.209(0.798-1.833)) or OS(P=0.391, HR=1.604(0.545-4.721)).
Discussion
In this study we found the optimal cutoff of prolymphocytes percentage was 1% which is different with previous study(Oscier et al. 2016). That may be due to that we choose TTFT as the endpoint. Besides, about prolymphocytes percentage was not statistically significant in multivariate analysis, we guess that may be attributed to that the sample was too little or there were only Chinese patients in our cohort. In conclusion, prolymphocytes percentage has certain prognostic significance in CLL patients and we think multivariate analysis would be different after we expanded our cohort.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal